A Cure for HIV?
A breakthrough regarding one of the most notorious viruses in modern times.
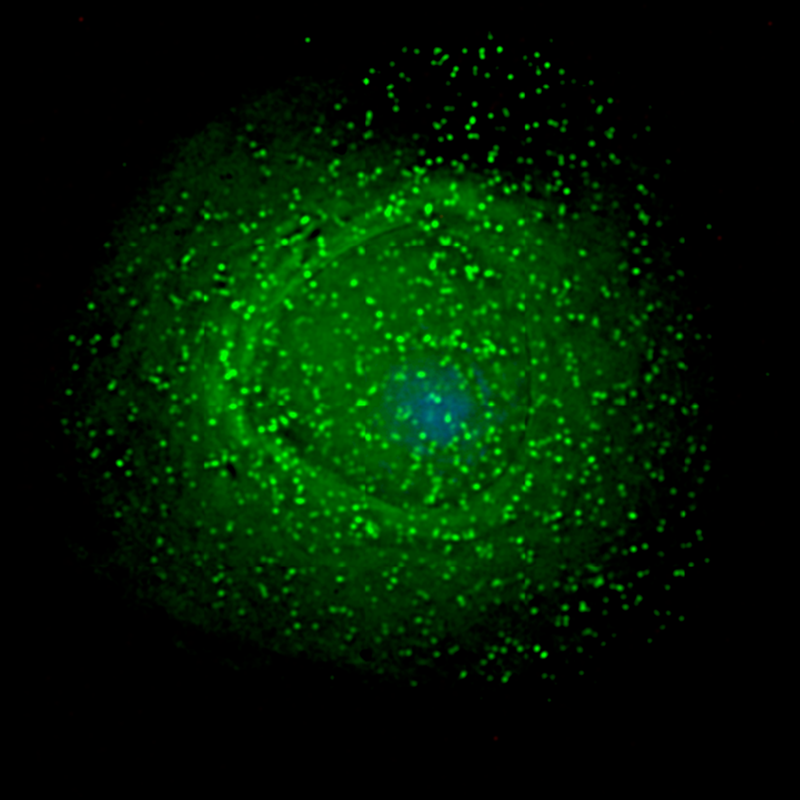
Photo by Creative Commons
Viral particles assembling around an infected immune cell.
A recent report came out early this week alleging that researchers have been able to “cure” a patient infected with HIV. This is only the second ever known instance of this virus being made undetectable in the body, the first being Timothy Ray Brown, dubbed “The Berlin Patient”.
Brown, after undergoing two bone marrow transplants from a donor with a rare genetic trait to treat his cancer, has lived HIV-free for over a decade despite not taking antiretroviral therapeutic drugs.
This new anonymous patient, dubbed “The London Patient” underwent an extremely similar procedure. He too, underwent bone-marrow transplants to treat cancer. The bone-marrow; however, contained a rare mutation known as delta 32.
This mutation controls the production of the CCR5 protein which exists on the surface of immune cells; HIV often requires this protein for infection and modification of the gene has allowed these two patients to be effectively cured from the virus.
It is interesting to add that the CCR5-related gene was the focus of another recent high-profile research case. In November of 2018, it was announced that a gene-editing tool CRISPR was used to edit human babies (twins known as Lulu and Nana) in Shenzhen, China.
According to He Jiankui, a scientist involved with the project, CRISPR was used to edit the CCR5 gene, allowing the twin girls to be resistant to HIV infection. This announcement was met with uproar from the scientific community regarding the medical and scientific ethics involved with editing the human genome with such new technology.
It should be noted that some scientists are wary of calling this new second patient situation a “cure”. Many are more conservative, calling it a remission. Though it is undoubtedly a breakthrough in the field of medical genetics and virology and a model for future work, the research is extremely rudimentary.
Additionally, it is unclear if this will ever be an option for HIV-positive individuals. The process of bone-marrow transplant is extremely dangerous and possibly life-threatening while living with HIV is not, bringing in the topic of ethics and reasoning. The two patients who were treated in this manner were being treated not for their HIV, but for their cancer. Regardless, this is a huge step in the right direction and a great demonstration of the rapidly advancing field of science.